Remember a few weeks ago when I argued that you should be vigilant and engaged in supporting scientific progress and condemning unscientific policies, regardless of your political leanings?
Well, I’m holding myself to the same standard. So when word spread this week that the U.S. House of Representatives passed a sweeping bill called the 21st Century Cures Act that has huge implications for the biomedical industry, I figured I should educate myself about it and share what I’ve learned with anyone who’s willing to listen.
The Cures Act has widespread bipartisan support and passed in the House with a huge majority, 392 to 26. It is expected to also sail through the Senate and be signed into law by President Obama, who is a strong backer.
And yet experts in healthcare and biomedicine are still arguing about whether it’s really aimed at benefiting patients or drug companies. More importantly, they’re divided on whether it will improve or undermine medical care in the U.S.
Here’s what I’ve learned so far about the bill, with the disclaimer that I’m not an expert on healthcare or politics. Unlike most of the media, I’m skipping the snappy quotes and emotionally charged rhetoric to simply lay out the facts as best I can.
The basics
The ostensible goal of the Cures Act is to advance biomedical innovation and get medical treatments to patients more efficiently. Even in our brutally divided country, these seem to be goals that (in theory) most everyone can agree on.
But not everyone agrees on how to get there. Republicans think the solution is easing FDA regulations for getting medical therapies to patients, whereas Democrats believe in increasing funding for medical research and treatment. The bill has such strong bipartisan support because it contains a hodgepodge of provisions that falling under these two umbrellas. It has something for everyone—which, in Congress, is not always a good thing.
Let’s take a look at the specific policies included in the bill.
Funding medical research and treatment
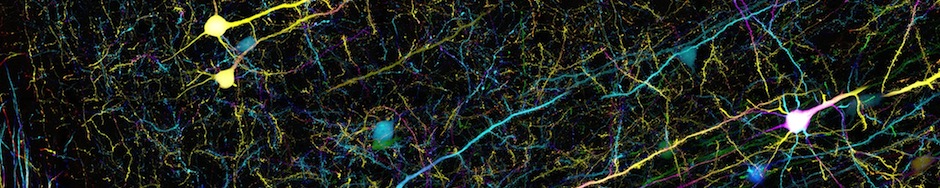
The Cures Act would provide $4.8 billion in biomedical research funding, which would go toward three large-scale programs: the Cancer Moonshot, the BRAIN initiative, and the Precision Medicine Initiative.
This all seems like money well-spent. As I argued in my previous post, funding biomedical research is one of the best returns on the dollar that taxpayers can get. And it’s not like curing cancer, understanding the brain, and tailoring medical treatments to patients are obscure areas of research; they address issues that directly affect nearly all of us.
In addition to funding biomedical research, the bill also contains provisions to promote mental health. It provides $1 billion to the states to fight opioid addiction, which has sharply risen in recent decades and has now reached crisis levels. The bill also strengthens the enforcement of a law that requires insurers to cover mental illnesses just like any other disease.
Where does the money come from?
It’s worth noting that most of this funding isn’t actually guaranteed. It falls under discretionary spending rather than mandatory spending, so Congress will have to vote each year to make the money available.
It’s also worth noting that the amount of money allocated for research has decreased by nearly half from a previous version of the bill that passed in the House. This decrease represents a compromise between Democrats who insisted on including research funding and Republicans who balked at any increases in federal spending.
Lawmakers reached a compromise by decreasing funding as well as agreeing to pay for some of the new spending by drawing money from prevention programs in the Affordable Care Act (ACA). These programs do things like discouraging kids from smoking.
Under normal circumstances I’d be highly skeptical of taking money away from these programs, and so would most Democrats—except that the ACA may soon be repealed under a Trump presidency anyway, which is apparently what spurred Democrats to make this compromise.
Easing FDA approval requirements
Ok, so far the Cures Act may not be a total slam dunk, but it should seem pretty appealing to anyone who supports more research funding and mental health treatment. That’s why most Democrats, including President Obama, are generally pretty happy.

Sen. Elizabeth Warren sharply criticized the Cures Act for its “huge giveaways” to the drug industry. (from youtube.com)
But then we get to the bill’s provisions regarding FDA approvals, which is where things start to get hairy. In order to get drugs and medical devices to patients more quickly, the Cures Act would weaken FDA requirements for evaluating and approving these therapies.
Easing requirements for drug approval should rightly raise some suspicions. The fact that pharmaceutical companies have been lobbying like crazy for the bill’s passage has provoked even more skepticism. A lot of the bill’s opposition centers on the idea that it’s basically a massive handout to the pharmaceutical industry.
Let’s look more closely at the proposed changes to FDA regulations.
“Real world” evidence isn’t better than science
Several of the bill’s provisions are aimed at repurposing existing, approved drugs for new uses. For instance, a drug called tamoxifen that was originally approved to treat breast cancer in 1977 was later found to help patients with bipolar disorder. There are lots of examples of drugs that turn out to be useful in multiple different contexts. In theory, it’s a good idea to efficiently repurpose drugs that have already been tested for safety.
But the Cures Act takes this idea to an extreme. To streamline the repurposing of existing drugs, the bill significantly lowers the bar for showing that a drug is effective in treating a new condition.
The gold standard for demonstrating a drug’s effectiveness is a randomized controlled trial. You randomly divide a group of patients into two groups, give half the patients a drug, give the other a placebo (pill with no active drug) or another form of non-treatment, and then compare the two groups.
Randomized controlled trials are an essential component of medical research. I can’t emphasize their importance strongly enough.
So many factors can affect a patient’s health, and it’s hard to know what made the difference in any individual case. Patients can get better on their own. They sometimes get better when they take a sugar pill or start seeing a new doctor, even if the treatment doesn’t change. Properly controlled clinical trials are the only way we can definitively ascribe any improvement in a patient’s health to the medical treatment he or she has received.
The Cures Act undermines this idea of randomized controlled trials as the gold standard for evaluating medical therapies. The bill allows drug companies to evaluate the effectiveness of a treatment by using “real world” evidence, which is defined as anything other than a proper clinical trial. This most commonly includes simply observing individual patients without any sort of control group, which can easily lead to spurious conclusions.

Types of medical studies, from Vox. The Cures Act would allow case reports and other types of observational studies to replace clinical trials for approving certain drugs.
Show me the data
Another way in which the Cures Act loosens FDA regulations is by allowing pharmaceutical companies to submit “summary-level reviews” rather than raw data when applying to approve a drug for a new use.
“Raw data” encompasses everything that was recorded in a study, like each patient’s blood test measurements or scores on a memory test. “Summary data” is much more limited; it refers to derived values like the average or standard deviation of these scores.
I spend most of my days looking at raw data, as do most scientists I know, and we can all tell you that raw data and summary data are two VERY different things. For example, summary data might tell you that the average score on a memory test for a group of 20 patients after drug treatment is better than before treatment. But the raw data might show that if you look at each patient individually, only 1 out of the 20 patients showed a huge improvement and the other 19 didn’t improve at all. Or maybe several patients got better but a few got significantly worse. Do we really want those scores averaged out?
Are “breakthroughs” worth the risk?
In addition to bypassing clinical trials in some cases, the Cures Act would streamline the approval process for high-risk medical devices that are classified as “breakthrough” devices. These devices would be allowed to undergo an expedited review to potentially get to market more quickly.
The problem is that the requirements for classifying a device as a “breakthrough” are fairly vague, and some argue that the bar for a “breakthrough” is set too low, not even requiring the device to provide “clinically meaningful” benefits.
At least one study has shown that faster approval of high-risk medical devices is associated with a higher probability of harm to patients, even including injury or death. So it seems to me like we should be exceedingly careful about which devices, if any, are allowed to go through an expedited review process.
Is faster really better?
What I’m telling you is that numerous policies in the Cures act would significantly lower the bar for evaluating whether a drug or medical device is safe and effective. In my opinion, this is simply irresponsible. And it’s certainly not the key to reforming American healthcare. There’s no evidence that the FDA is really the bottleneck that prevents patients from getting drugs that they need.
Nevertheless, I do think it’s worth discussing whether it’s actually possible to improve the FDA approval process to bring valuable treatments to patients more quickly. Pharmaceutical and medical device companies have long complained that the FDA approval process is too burdensome and costly. Of course, they’re hardly unbiased. But do they have a point?
In a word, no. In fact, the FDA is already one of the fastest regulatory agencies in the world. Nearly all applications for new drugs are approved in six to ten months, which is pretty efficient given the complexity and importance of the process. Over two-thirds of drugs are approved based on studies lasting 6 months or less—again, a pretty reasonable time frame.

Median approval time for new drugs across different regulatory agencies, showing that the FDA is faster than its counterparts in Europe (EMA), Japan (PMDA), Canada, Switzerland, and Australia (TGA). (credit: Regulatory Affairs Professionals Society)
We may just have to accept that carefully evaluating a drug’s safety and efficacy takes time, and you generally can’t speed up the process without compromising its integrity. Moreover, the FDA already has the tools and authority to streamline access to drugs, especially in crises such as the AIDS epidemic of the 1980s, and has been steadily moving in that direction on its own.
For instance, the FDA has moved toward evaluating treatments based on biomarkers and other “surrogate endpoints” rather than clinical outcomes. Here’s an example of what that means. The best way to evaluate whether a cancer treatment is effective is to determine whether patients are healthier and live longer after treatment. A faster and easier way to evaluate the effectiveness of the same treatment would be to measure whether the tumor shrinks or disappears. This is called a “surrogate endpoint” because it’s not what we ultimately care about, but it’s correlated with the patient’s health and longevity.
Not everyone agrees that these kinds of shortcuts are a good idea. They may lead to a system where drugs are more readily available, but less effective. One study found that the effectiveness of cancer drugs that were approved based on surrogate endpoints is still largely unproven.
So when it comes to approving medical therapies, I’m inclined to think that we don’t want to take shortcuts—no matter how tempting they might seem.
What about the cost of healthcare?
Many people argue that the core problem with the American healthcare system is its cost. So we should all be asking whether the Cures Act will do anything to decrease the cost of healthcare. The answer is unclear.
Pharmaceutical companies argue that if the FDA approval process becomes less burdensome, then their costs will decrease and that savings would be passed on to consumers. Of course, everyone who’s not a pharmaceutical company is rather skeptical that those companies would have the faintest interest in passing on their cost savings to the rest of us.
On the other hand, if ineffective drugs make it to the market because of looser FDA regulations, this would clearly impair the cost-effectiveness of medical treatment—raising costs without improving health.
So it’s not clear to me how the bill will impact healthcare costs. Mostly I have to agree with politicians who criticize the Cures Act for failing to address this issue directly. If we truly want to improve medical care in this country, bringing down the bloated costs of U.S. healthcare is one of the most important things we should be focusing on.
The verdict
This bill is a mixed bag. My first instinct was that it can’t be that terrible if it’s got such widespread bipartisan support. But my final verdict, after hours of research, is that it seems like a pretty bad idea. At least some healthcare experts agree.
I’d need a deeper understanding of how the FDA works to be 100% sure that the bill would significantly undermine our drug approval process, and that those negative consequences would outweigh the benefits of enhancing research funding and mental health treatment. But overall, I think it seems like a poor deal for patients. We’re getting a relatively small, temporary increase in research and medical funding in exchange for severely undermining the FDA’s regulatory standards.
If you agree with me, there’s still time to express your opinion to your senators and President Obama. Some prominent senators such as Elizabeth Warren and Bernie Sanders have spoken out strongly against the bill, which may give the opposition some traction.
But it seems pretty likely that this bill will become law, for better or worse, and I hope this post gives you a greater understanding of its sweeping consequences. There are other issues entwined in this debate that I didn’t get a chance to discuss, and I’m sure there are subtleties that I don’t completely understand, so if you’d like to point out anything I missed please comment below!
Key sources for this post:
Regulatory Affairs Professionals Society: “Regulatory Explainer: 21st Century Cures Redux and What it Will Mean for FDA” (the most complete and unbiased summary that I found)
STAT: “House approves the 21st Century Cures Act, sending landmark bill to Senate”
NPR: “Congress Poised To Pass Sweeping Law Covering FDA And NIH”
Vox: “House lawmakers passed the biggest health reform bill since the Affordable Care Act”
Vox (article from 2015): “This new bill would add $9 billion for medical research. Here are 5 reasons critics are terrified.”
New York Times: “$6.3 Billion Measure Aims to Cure Ailing Health Care Policies”
US News and World Report: “Congress Poised To Pass Sweeping Law Covering FDA And NIH Latest Version of Drug and Device Overhaul Bill Doesn’t Satisfy Critics”
Health News Review: “21st Century Cures Act nears passage with little news media scrutiny”
Health Affairs Blog: “The Current 21st Century Cures Legislation Is Still A Bad Deal For Patients”

Incredibly interesting reading about this current affair within the US. It will be fascinating to follow this into the new year to indeed see how this issue will affect the US in the months/years to come.
most informative article I found on the subject, yet it seems that very few have seen it! Shared